Ireland’s average health system
“The Irish lifestyle may be fun but there’s no way you can describe it as healthy,” according to the head of the OECD’s health division Mark Pearson. Meadhbh Monahan reports.
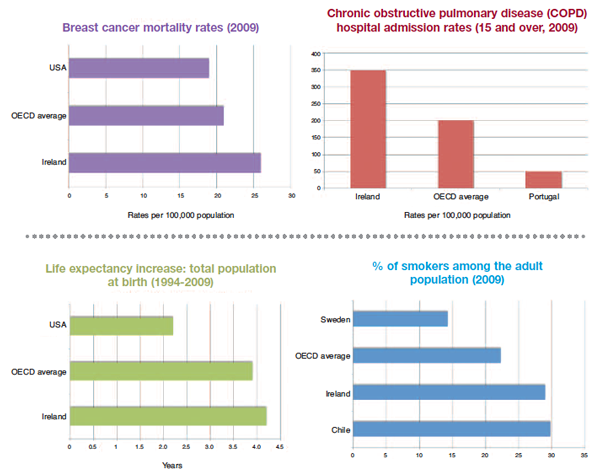
Ireland has had “stunning” increases in life expectancy (with the age of the total population at birth increasing from 76.6 to 80 years since 2000) but is “doing badly” at preventing and treating chronic conditions, which are largely self-inflicted through lifestyle choices. Mark Pearson brought this message to the ESRI Budget Perspectives event.
While Ireland’s health spend per capita rose quicker than the OECD average during the boom years (at a rate of 7.6 per cent rate compared to the overall OECD rate of 4 per cent), it now spends the same as the OECD average (9.6 per cent of GDP). Total expenditure in 2010 was €14.8 billion and the 2011 estimate is €14.1 billion. However, this money is not being used efficiently, Pearson warned.
“If Ireland was as efficient as the most efficient OECD countries it would spend what it currently spends and have three more years of life expectancy,” he stated.
The health expert added that an alternative would be to retain current life expectancy, spend less and become more efficient. “It’s not so easy to relate that into policies,” he conceded.
An increasingly ageing population across Europe up to 2025 is set to raise the heath spend required by 2.5 per cent of GDP, the OECD predicts.
While Ireland’s proportion of daily smokers has decreased from 45.6 per cent in the early 1970s, at 29 per cent, it is still well above the OECD average of 22.3 per cent. Ireland is fourth highest in the OECD countries (after the Czech Republic, Austria and Estonia) in terms of its alcohol consumption which stands at 11.3 litres per adult, compared to the OECD average of 9.3 litres. Obesity levels in Ireland are the same as the UK (23 per cent) which, again, is above the OECD average of 21 per cent. Growing levels of obesity and an unhealthy lifestyle “foreshadow” more chronic diseases and will lead to higher health care costs, the health analyst warned.
On the contentious issue of the closure of hospital beds, Pearson argued that if campaigners against local hospital closures really cared about the quality of service, “they’d be demonstrating insisting that their local hospital is closed down because local hospitals can’t do a lot of these complicated procedures as well as big hospitals.”
He cited data from the Netherlands on cystectomy operations which found that if a hospital does 10 or more operations per year, the mortality rate is 1.2 per cent, if it does five or more the rate is 3.6 per cent and if it does less than five per year the mortality rate increases to 6.4 per cent.
Ensuring that unnecessary hospital admissions are avoided is essential if the system is to be improved because it costs €50 to visit a GP as opposed to €1,000 to spend one night in hospital. Ireland needs to consider new ways to incentivise primary care so that chronic conditions such as diabetes do not require unplanned trips to the hospital.
Currently, Ireland pays for the amount of activity doctors do “rather than the health they deliver.” It should follow the lead of other OECD countries and experiment with pay-for-performance, Pearson suggested. For example, Germany combines rewarding doctors for health delivery with clinical guidelines.
Pearson concluded: “Basically, one reason why you are doing average in health is because the health system hasn’t tackled lifestyle issues very well.”